
One of the most frequent visitors to my outpatient clinics is the patient with awareness of their heartbeat or ‘palpitations’.
This blog is aimed to give you an understanding of the physiology behind your symptoms and I have deliberately not made it a long list of causes of palpitations, as I think it is more important that you understand what to expect from your body. I have provided links for further reading at the end of the article.1-5
What is a palpitation?
A palpitation is a noticeably rapid, strong, or irregular heartbeat due to agitation, exertion, or illness. It may make you feel like your heart is beating too hard or too fast, skipping a beat, or fluttering. It may be felt in your chest, throat, or neck. Usually palpitations are not serious or harmful and often go away on their own. Quite often a palpitation will have settled completely by the time the patient gets an appointment!
You may wonder ‘Why am I not always aware of my heartbeat?’ – it’s because the body’s internal control mechanisms (autonomic nervous system) silently manages bodily functions such as this. It is only when your threshold of awareness lowers that you notice your normal breathing or hear or feel your normal heart beat.
What might cause palpitation?
Most of the time palpitation are due to stress and anxiety, lowering your threshold of awareness. Too much caffeinated drinks, nicotine, might cause palpitation by raising adrenaline levels in the body and alcohol has a direct toxic affect. Pregnancy is another common cause in women, due to the increased blood circulation.
The normal heart beat
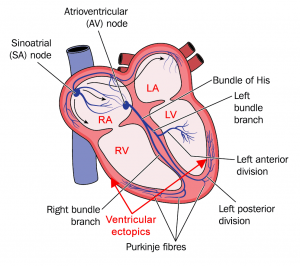
Sinus rhythm is the name given to the normal rhythm of the heart where the heart beat is initiated from the heart’s internal pacemaker or sinus (sinoatrial) node. It is initiated as an electrical impulse that is then conducted across the heart via a junction box (atrio-ventricular node) and fast fibre connections (Bundle of His) to the main pumping chambers, or ventricles.
The blood is then pumped out from the ventricles at high pressure through arteries. Your arteries are elastic, so stretch when blood passes through them and then recoil afterwards, helping to push the blood around the body. It is this that forms the pulse that is felt when you compress an artery against a structure such as the bones at the wrist, or the vertebrae in the neck. If the pulse pressure is large, as in hypertension, or the rate is fast, then nerve endings in the surrounding tissues pick this up making you aware of the change in pattern.
Although the sinus node is the heart’s natural pacemaker, all heart cells can initiate electrical impulses. The atria and ventricles can therefore independently generate impulse (see arrows in diagram) leading to ectopic beats, or an abnormal circuit can be set up between cells, leading to abnormal patterns of heartbeats.
Abnormal heartbeats – arrhythmias
If the heartbeat pattern is abnormal it is often called an arrhythmia (sinus arrhythmia, however, refers to the normal increase in heart rate that occurs each time you inhale, or breathe in).
If everyone were fitted with a monitor to record their heartbeat, doctors would not be surprised to find extra beats going unnoticed and even silent benign arrhythmias.
When should you seek medical attention?
The majority of patients referred with palpitation either do not have an arrhythmia or the arrhythmia is clinically insignificant. Only in rare cases is the palpitation a sign of a more serious problem. It is sensible to seek immediate medical attention if your palpitation is associated with shortness of breath, dizziness, fainting or chest pain.
Monitoring and referrals
I usually ask my patients to tap out their abnormal heartbeat with their hands on their chest or the desk to clarify the rate and also give me an idea about regularity or otherwise.
A 24-hour tape (an ambulatory rhythm monitoring or ARM) is often requested by your doctor, but to be useful, you need symptoms at least three-to-four times per week to make 24-hour monitoring a sensible choice. Given a history suggestive of extra beats (ectopy) and without additional risk factors, you do not necessarily require monitoring.
The anxiety generated in some people with new symptoms prompts a referral to their GP and if they do not give a satisfactory explanation, or instill confidence, a referral to a cardiologist for a second opinion is inevitable. Often I am referred patients after a practice nurse picks up an irregular pulse (unnoticed by the patient) when taking blood pressure in a routine health check and this sets off a referral that could be avoided with appropriate screening in the practice. A rhythm strip, an ECG trace easily done by the nurse, can exclude the more dangerous irregularities or reassure the patient if they were just ectopics. Many patients now record their own heartbeat on smart watches and smart phones!
Tests and examinations
Slow heart rates (bradycardia) may be normal in athletes (including varying degrees of heart block), and a fast heart rate (tachycardia) is a normal finding in pregnancy, but an ECG will detect these. Often symptoms occur during exercise so tests such as an exercise test (ETT) can be used to mimic this to provoke and catch them. A cardiac ultrasound or ECHO is an essential test that looks for structural heart disease.
Your nurse or GP will take your medical history to see if there are any high risk factors and may order baseline tests to find the cause if indicated – such as thyroid hormone levels to exclude an overactive or underactive thyroid. I won’t list these here but the links below will help guide you. A full cardiac examination including blood pressure and listening to your heart (for murmurs) is essential and can be done by a GP or sometimes an experienced specialist practice nurse. A major health target currently is to detect atrial fibrillation (an irregular and often abnormally fast heart rate), as treatment can prevent stroke. High-risk patient groups are identified (e.g. those with previous transient ischaemic attack or TIA, previous stroke “CVA”, hypertension, alcohol excess and the elderly [more common over 80yrs]) and offered an ECG to screen for this arrhythmia.
Management
If there’s no underlying cause, lifestyle changes can help, including stress management, however the benefit of regular modest exercise cannot be underestimated. Avoiding excess alcohol and avoiding dehydration are useful extra tips.
Doctors use the traffic light system shown below to guide management and patient care:6
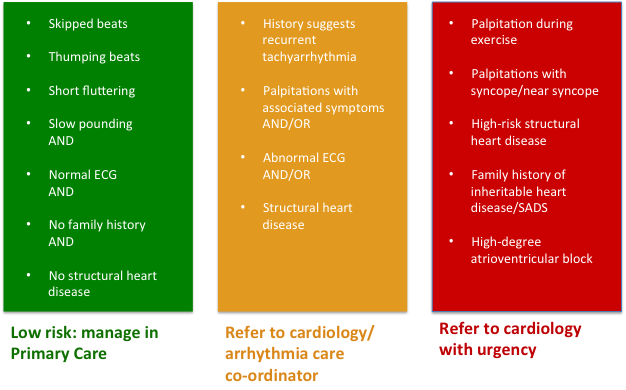
Reference: Wolff A et al 20096
With the advent of ‘Choose and book’ the referral process has become more complex, but offers the opportunity to speed up the patient’s journey by advising the patient of the most appropriate provider. Telemedicine is also a very useful tool in my armory and I have reassured many patients or confirmed a diagnosis using this service.
This article is for information only and should not be used for the diagnosis or treatment of medical conditions. myHealthSpecialist makes no representations as to the accuracy or completeness of any of the information in this article, or found by following any link from this article. Please consult a doctor or other healthcare professional for medical advice.

Dr Lance Forbat, Consultant Cardiologist
“Heart2Heart” Doctor