What is Torsades de Pointes?
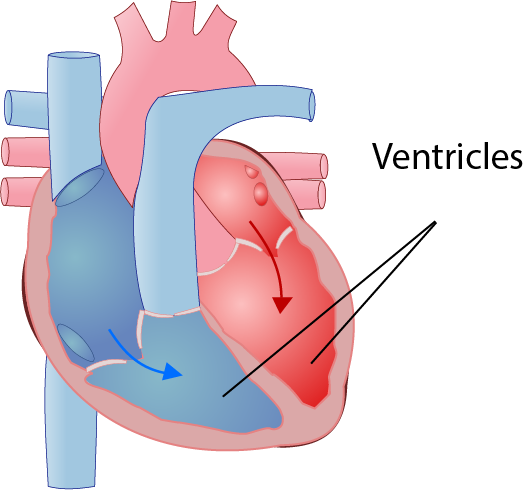
Torsades de Pointes (TdP) is a heart condition that is caused by a change in the electrical activity in the heart causing it to beat abnormally. TdP is a specific type of electrical activity that particularly affects the ventricles (the larger chambers in the heart), causing them to contract too quickly. This condition is identified using an ECG (electrocardiogram; monitoring that shows the electrical activity in the heart). Torsades de Pointes literally means “twisting of the points”, which describes the classical pattern seen on the ECG. TdP can resolve on its own, giving symptoms of palpitations, dizziness or collapse, but, if not treated, TdP can stop the heart working and result in sudden cardiac death.
How do people get TdP?
The ECG below shows what’s known as a ‘QT interval’ – this represents the electrical activity of the ventricles:

If the QT interval is longer than normal (i.e. it takes longer for the electricity to travel through the ventricular conduction system), the risk of developing TdP is increased. Women normally have a slightly longer QT interval than men. A longer QT interval can also be something you are born with or caused by other medical conditions or abnormalities:
- Congenital Long QT Syndrome
- Cardiac problems
- Other heart problems that are associated with prolonging the QT interval and increasing the risk of developing TdP include:
- Medications
- There are several medications that can prolong the QT interval, including[vii]:
- Drugs to treat arrhythmias (electrical problems in the heart)
- Several antibiotics and antifungals
- Antidepressants like citalopram or amitriptyline
- Some medications that are used to treat other psychiatric disorders
- Some anti-sickness medications like ondansetron
- If you have any concerns regarding any of the medication you are taking, you should discuss this with your GP
- There are several medications that can prolong the QT interval, including[vii]:
- Electrolyte imbalance
- Very low levels of the following electrolytes can cause TdP:
- Potassium
- Calcium
- Magnesium
- Very low levels of the following electrolytes can cause TdP:
These are often caused by severe or prolonged vomiting and/or diarrhoea or severe malnutrition, but can also be caused by some types of endocrine disorders.
- Other
How do you treat TdP?
Treatment of TdP depends on whether someone is currently having an episode of TdP or generally at risk of developing TdP (i.e. they have risk factors that mean they have a long QT interval).
Immediate treatment:
- People with TdP are treated following national resuscitation guidelines
- If they are in hospital this involves:
- Removal of anything that could have triggered the TdP (such as QT interval prolonging drugs)
- Defibrillation
- Administration of magnesium sulphate
- Correction of any abnormal heartbeat or electrolyte imbalance, sometimes using drugs or ‘pacing’ (taking over the electrical activity of the heart)
- If they are not in hospital, the normal basic life support guidelines should be followed:[xiii]
- Ensure it is safe to approach the victim
- Promptly assess the unresponsive victim to determine if they are breathing normally
- Be suspicious of cardiac arrest in any patient presenting with seizures and carefully assess whether the victim is breathing normally
- For the victim who is unresponsive and not breathing normally:
- Dial 999 and ask for an ambulance. If possible stay with the victim and get someone else to make the emergency call
- Start CPR and send for an AED (automated external defibrillator) as soon as possible (there should be one in most public places with clear, simple instructions for use)
- If trained and able, combine chest compressions and rescue breaths, otherwise provide compression-only CPR
- If an AED arrives, switch it on and follow the instructions
- Minimise interruptions to CPR when attaching the AED pads to the victim
- Do not stop CPR unless you are certain the victim has recovered and is breathing normally or a health professional tells you to stop
Long-term treatment:
- For people with congenital LQTS, the following is recommended[xiv]
- Ensuring a good diet with enough hydration and a variety of fruits and vegetables (to avoid any electrolyte imbalances)
- Avoidance of any drugs that could cause a longer QT interval
- Beta-blockers (such as propranolol)
- Permanent pacing with an ICD pacemaker (Implantable Cardioverter Defibrillator)
- If these treatment options are not working well enough, or the person is at a high risk of developing TdP, they can have an operation called a ‘Sympathectomy’ to help control the heart’s rhythm[xv]
- For people without congenital LQTS, the following is recommended:
- Ensuring a good diet with enough hydration and a variety of fruits and vegetables (to avoid any electrolyte imbalances)
- Correction of any reversible risk factors that could cause long QT interval
- In cases where these factors cannot be avoided, or in the case of other heart rhythm problems, pacemakers can be implanted to prevent TdP
This article is for information only and should not be used for the diagnosis or treatment of medical conditions. myHealthSpecialist makes no representations as to the accuracy or completeness of any of the information in this article, or found by following any link from this article. Please consult a doctor or other healthcare professional for medical advice.

Dr Raj Khiani, Consultant Cardiologist
Book an appointment with Dr Raj Khiani

Bethan Tyler
Final year medical student, Kings College London